What You Need to Know About Early Detection
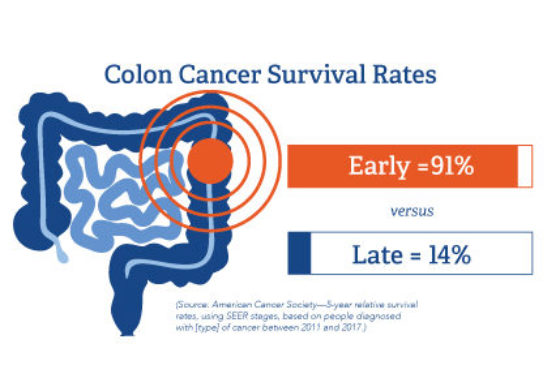
Gastrointestinal cancers are on the rise; however, they are survivable when detected early. When colon cancer is diagnosed at stage 1, patients have a 91% survival rate; when diagnosed at stage 4, the survival rate drops to 14%. DetecTogether’s 3 Steps Detect education creates awareness and gets people to the doctor, so doctors can conduct necessary exams and diagnostics in a timely way. Putting off addressing symptoms is never a good idea. If it’s cancer, cancer doesn’t cure itself and delaying diagnosis only allows it to get worse.
Insights & Advice
Q&A with MGH’s Christopher Velez, M.D.

DetecTogether sits down for a Q&A with Christopher Velez, M.D., of the Department of Gastroenterology at Massachusetts General Hospital in Boston, Mass. Gastroenterologists are medical doctors with a specialty in diseases of the digestive system—from the mouth, to esophagus, stomach, pancreas, bile ducts, gallbladder, liver, small and large intestines.
Absolutely. Step 1 is when you’re feeling well, and you’re getting your screening colonoscopy, your virtual CT-colonoscopy or your stool-based FIT or Cologuard tests. That is perhaps the most important aspect of step one.
Step 2; if you’re starting to notice any rectal bleeding, or you’re starting to lose weight without trying, call your doctor.
Step 3; seek care from a provider. This is where you need to be your own hero, be your own advocate and bring your concerns to their attention. Doctors are often very pressured for time. Primary care doctors have a load of responsibility that they have to shoulder when it comes to patient care. It may be tempting not to raise your concerns and say I’ll just wait until the next visit because the doctor seems very busy.
No, be your own advocate and say, “Actually, there’s an important thing I want to discuss that’s concerning me. I’m losing weight. I’m having some bleeding. And by the way, I have a family member who had colon cancer. Do I need to be worried about that?”
Dr. Velez: Colon cancer is the primary gastrointestinal cancer that we worry about. Colorectal cancer is a disease that is preventable through screening. Screening is what you do when you are feeling “great,” DetecTogether’s Step 1, when you are not having symptoms. We worry about esophageal cancer sometimes in patients. We worry about stomach cancer sometimes. But our first and foremost concern when it comes to cancers of the GI tract is colorectal cancer.
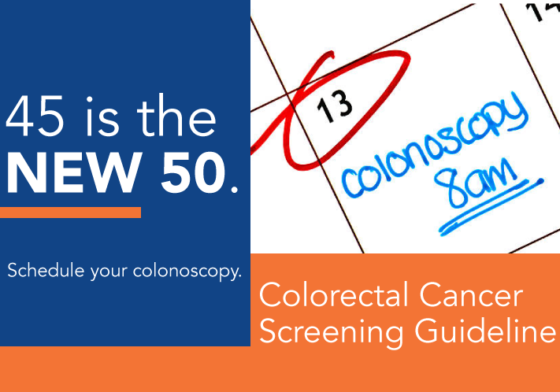
The overall concern over the past 10 to 15 years with colon cancer is twofold. First, we are noticing that younger and younger people are being diagnosed with colon cancer. So that’s part of the reason why, when people are feeling totally okay, we recommend that they start their colon cancer screening at age 45. Most people may be aware of the original recommendation of starting at age 50, but we’re recommending earlier screening at age 45. Because younger and younger patients with cancer are being diagnosed.
There are also disparities that exist between different groups, ethnic and racial minorities in particular have lower rates of screening, and they tend to have worse colon cancer outcomes. We are increasingly realizing that there are disparities in the way that we deal with colon cancer in the US healthcare system.
- There’s a difference between screening colonoscopy, which you do when you’re feeling great, and diagnostic colonoscopy. We recommend screening colonoscopy for people when they hit age 45. This procedure allows us to detect polyps and remove them. That’s how we can help prevent colon cancer.
- Some people are squeamish about the idea of having a camera inserted through a colonoscopy especially if they’re not feeling bad. The point of screening is to go before you get feeling bad. You can find it, take care of it, and keep on feeling great.
- For those who are really squeamish, there are stool-based tests like Cologuard. If you don’t do it at a regular frequency, however, you may miss a cancer. Nothing can be removed early, it only detects the presence of cancer or more advanced polyps.
- One other option is an annual test called the FIT test. It looks at microscopic amounts of blood that are present in the stool, which can be associated with large polyps or cancer. Polyps are growths that then become cancer, or microscopic amounts of blood that can be found if cancer is already present. The downside of that is it needs to be done annually. Sometimes, people in my experience get their first one, get their second FIT test, and then once they have a negative, they stop following the recommendations.
- There’s also the virtual colonoscopy or a CT colonography, where you drink large amounts of medication to clean your colon out. But you go to a radiologist’s office and they inflate the colon like a balloon. And then they look to see on imaging if there’s anything concerning like a polyp or a cancer.
- It is important to note for the non-procedure colonoscopy, most times when there is a positive test, you end up needing to have the colonoscopy in the end.
Every type of test has its miss rate. It has its false-positive rate, meaning it says that there’s an issue even though there isn’t anything there. And it’s important to understand why we recommend certain tests. And if you’re going to do them, they’re all deemed to be equivalent if you follow the instructions for screening.
I prefer colonoscopies, but most important is that NO MATTER HOW YOU DECIDE TO GET TESTED AND/OR SCREENED FOR COLON CANCER, MAKE SURE THAT YOU GET TESTED AND SCREENED FOR COLON CANCER. Pick the test that’s right for you.
Fear. I’ve seen patients that have a family history of colon cancer, and they are afraid they have it, but they’re so concerned about receiving a diagnosis of colon cancer that they don’t want to go in for the testing.
Misinformation. A lot of it is misinformation. It’s thinking, “Oh, the only way that you can screen for colon cancer is a colonoscopy. I don’t want to get that done. So I won’t undergo colon cancer screening when I’m feeling well.” That’s why I offer people the option, when appropriate, to get those other tests that I mentioned: the virtual colonoscopy, the Cologuard or the FIT testing.
Access. If people are from communities that are traditionally disenfranchised, for example, limited English proficiency communities, they’re less likely to get culturally competent care or language-concordant care. It may be that there is a disconnect between provider and patient. Sometimes it’s a question of access. Where people are uninsured and only recently have we, with federal regulations, mandated that screening procedures be covered by different insurance plans. But people may, if they’re deciding between paying rent or paying for their medications, it’s understandable why they would then not necessarily opt for what they view to be an optional test even though it’s not.
Be Proactive About You Health

Dr. Justin Maykel, Chief of Colorectal Surgery at UMass Memorial Health, and member of the DetecTogether Board of Advisors, shares usable knowledge with us as part of Colorectal Cancer Awareness Month. View his video series below.
Why Firefighters Should Get Screened
Research has shown that firefighters are 1.21 times more likely to develop colorectal cancer than the general public. It is crucial for members of the fire service to be aware of the early signs of the disease, seek medical attention if symptoms persist, and get annual screenings starting at 40. When detected early, colorectal cancer is more treatable and survivable.
Hear Mike’s Story
Eddie’s Afterglow
Delayed diagnosis cost Eddie McDonagh his life. His wife, Kimberly, reflects on their life together and shares his story to help other families avoid what happened to hers.
Hear Eddie’s Story